|
www.MathResolutions.com
Software Products for the Radiological Sciences
| Search |
|
www.MathResolutions.comSoftware Products for the Radiological Sciences |
|
| Home Page | Product Review | Program Manuals | Download Programs | Purchase | Site Map |
| Dosimetry Check | MarkRT (VGRT) | RtDosePlan | System 2100 | MillComp | C++ Library |
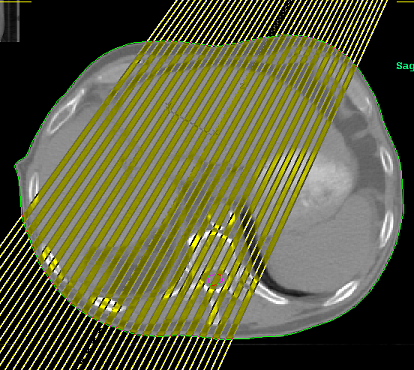
To compute the dose to the patient from a treatment portal,
pencils are first created that cover the treatment field and patient.
The area of a beam field is simply divided up into small pixels
(in a plane perpendicular to the beam), each pixel being a separate
pencil. Whether a pencil beam algorithm or a full superposition
algorithm, it is necessary to trace each pencil through the patient
as illustrated in the below image where we have lighted up every
other pencil.
 Typically the density of the
material the beam is going through is noted and one computes terma along
each ray. However, to compute the dose to the patient
one must know the intensity of radiation that reaches each ray.
Typically the density of the
material the beam is going through is noted and one computes terma along
each ray. However, to compute the dose to the patient
one must know the intensity of radiation that reaches each ray.
In a planning system to know the intensity that is reaching each pencil
on the surface
of the patient, a source model is used that can compute the intensity
down stream from the collimation system on any point on a plane
perpendicular to the central ray, as illustrated in the below
image.
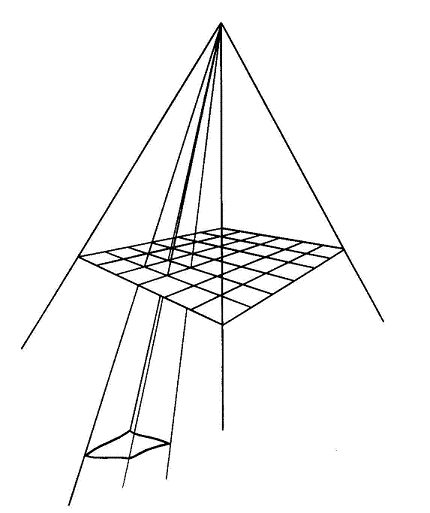 The source model must take into account everything, the flattening
filter, the collimator system, the multi-leaf system, wedges, and
any dynamic movements of those things to arrive at the final intensity
that reaches each pencil.
The source model must take into account everything, the flattening
filter, the collimator system, the multi-leaf system, wedges, and
any dynamic movements of those things to arrive at the final intensity
that reaches each pencil.
Dosimetry Check does not have a source model, which is the
whole point of Dosimetry Check. In Dosimetry Check, the
source model is replaced with a measured source model.
If you were to put a piece of x-ray film on the couch and expose to
the treatment portal straight down for the whole beam on time, you will
have a picture of the field intensity that takes into account everything,
such as leaf leakage, since you have just measured it all. In Dosimetry Check
you can use the EPID or a diode or ion chamber array for greater
convenience. The
distance to the patient surface for each pencil is known from the CT scans
and beam position.
Using x-ray film, the beam film (taken BEFORE or without the patient)
gets darker the more radiation a spot gets.
 As noted above, the port image without the patient in the beam is a
record of how much radiation each pixel gets.
As noted above, the port image without the patient in the beam is a
record of how much radiation each pixel gets.
It is necessary to convert this information to a unit that will
make it possible to compute the dose in centiGray to the patient
from each pencil. Each spot on the
image is mapped to the monitor units that would produce the same darkness
at the center of a 10x10 cm field size (i.e. the field size that you
calibrate the accelerator to).
We call this resultant number the "relative monitor unit" (RMU).
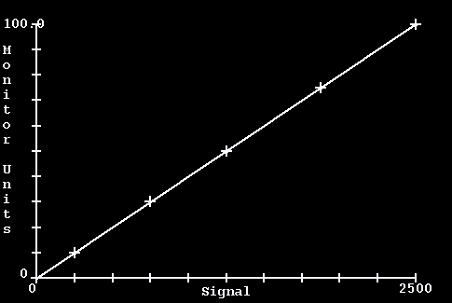
If you calibrate your machine with a 10x10 cm field size, you would use
that field size to run a calibration curve. For open fields, the
RMU value would be the monitor units for the beam times the scatter
collimator factor for that field size. For IMRT fields, the RMU
can be thought of as the effective monitor unit at that location
within the radiation field. The RMU is then a measure of the
in air ray field intensity, in a unit we can use directly for
calculation of the dose to a phantom.
Hence we are effectively calilbrating in monitor units. To compute the dose to the patient we have to know what your definition of a monitor unit is. Some examples might be:
100 cm SSD, 10x10 cm field size, depth = 1.5 cm, 1.0 cGy/mu or 98.5 cm SSD, 10x10 cm field size, depth = 1.5 cm, 1.0 cGy/mu or 95 cm SSD, 10x10 cm field size, depth = 5.0 cm, 1.0 cGy/mu or 100 cm SSD, 10x10 cm field size, depth = 10.0 cm, 0.670 cGy/muBasically, what ever field size you set, SSD, depth, and dose you measure per monitor unit when you check the output of your linac would be your monitor unit definition. This definition has to be specified in your beam data in Dosimetry Check.
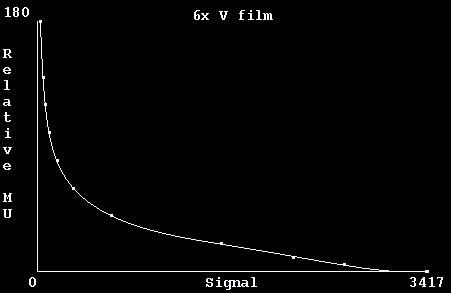 This curve is used to map the
pivel values on the beam images to RMU.
This curve is used to map the
pivel values on the beam images to RMU.
Once converted to RMU, Dosimetry Check can compute the dose from a
beam to the patient in centiGray.
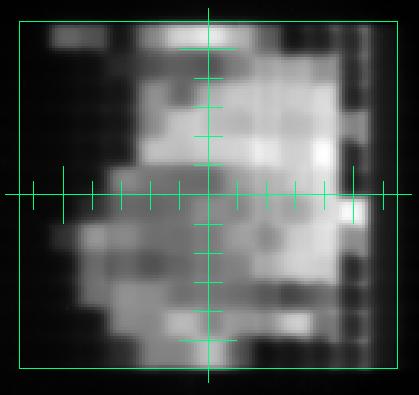 Here, zero RMU is black, whiter is larger RMU.
Here, zero RMU is black, whiter is larger RMU.
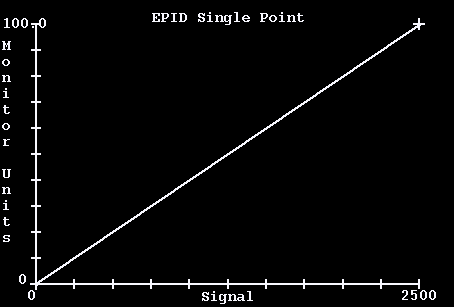
But an EPID or similar
device will generate internal scatter within the device. This
is corrected for by doing a deconvolution with the
spread function of the device to arrive at in
air fluence in RMU.
Shown below is an EPID image of a modulated field for a head
and neck case after mapping to RMU units (where white is more radiation).
The pixels on the RMU image are used as "weights" for the corresponding pencil beams. The fluence map that we have derived here from a calibrated image of the beam completely determines the dose to the patient. This process is similiar to how a planning system computes the dose, except here we are using the measured fluence instead of computing the same from knowledge and models of what kind of things modulate the beam. By starting with measurement instead of a model, we verify the dose and dose distribution that the patient receives.
The dose computed by Dosimetry Check may be compared directly to that
computed by the planning system.
 ADAC IMRT plan (green) versus Dosimetry Check (magenta) with inhomogeneity
corrections on, courtsey of Dr. Tianyou Xue.
ADAC IMRT plan (green) versus Dosimetry Check (magenta) with inhomogeneity
corrections on, courtsey of Dr. Tianyou Xue.